What the Meaning of Follicular Study Is for Your Fertility
- DeVeNdRa NaTh
- Dec 10, 2025
- 9 min read
When you're trying to get pregnant, timing can feel like everything. But how do you pinpoint that perfect window? That's where a follicular study, also known as follicular monitoring, comes in.
In simple terms, it’s a series of ultrasound scans that let us watch what's happening inside your ovaries in real-time. We're tracking the growth of the ovarian follicles – the tiny, fluid-filled sacs where your eggs mature. The main goal? To predict ovulation with incredible accuracy and boost your chances of conception.
What a Follicgular Study Really Means for Your Fertility
Think of it less like a medical procedure and more like getting a personalised roadmap for your fertility journey. While the technical side involves ultrasounds, the true meaning of a follicular study is the clarity and control it gives you. It takes the guesswork out of trying to conceive and replaces it with a clear, data-driven plan.
This "fertility roadmap" gives you a behind-the-scenes look at your own body. Instead of relying on apps or ovulation kits alone, you can literally see your follicles growing day by day and know exactly when your body is getting ready to release an egg. For many people, having this insight is incredibly empowering and can take a lot of the stress out of the process.
Who Benefits Most from This Fertility Roadmap?
Follicular monitoring isn't for everyone, but for some, it's a game-changer. It's particularly helpful for:
Couples Trying Naturally: If your cycles are a bit unpredictable, this helps time intercourse perfectly.
Individuals Undergoing IUI: It ensures the insemination procedure happens at the absolute peak of fertility.
Patients in IVF Cycles: It's essential for monitoring how your follicles are responding to medication and scheduling the egg retrieval at just the right moment.
By watching follicle growth and pinpointing ovulation, a follicular study provides the critical information needed to turn hope into a structured, well-timed plan, significantly increasing the odds of a successful pregnancy.
Your Step-by-Step Guide to the Follicle Tracking Process
Going through a follicular study for the first time might seem a bit daunting, but the process itself is quite straightforward. It’s all about giving you and your doctor a clear, real-time picture of your cycle.
Think of it like a gardener watching a flower bud. They check it every day, noting its growth, waiting for the perfect moment for it to bloom. That’s exactly what follicle tracking does for ovulation.
Getting Started: The Baseline Scan
Your journey starts with a baseline scan, which is usually done on day 2 or 3 of your period. This first scan is the starting line. It lets the doctor see your ovaries in their resting state, count the small follicles (called antral follicles), and make sure there are no cysts that could interfere with the cycle.
The Heart of the Process: The Monitoring Phase
After that initial scan, you’ll come in for a few more appointments, typically every other day or so. The main tool for this is a transvaginal ultrasound (TVS). It might sound intimidating, but it’s a quick and generally painless scan that gives the clearest possible view of your ovaries and uterus.
During each of these scans, your doctor is keeping a close eye on two critical things:
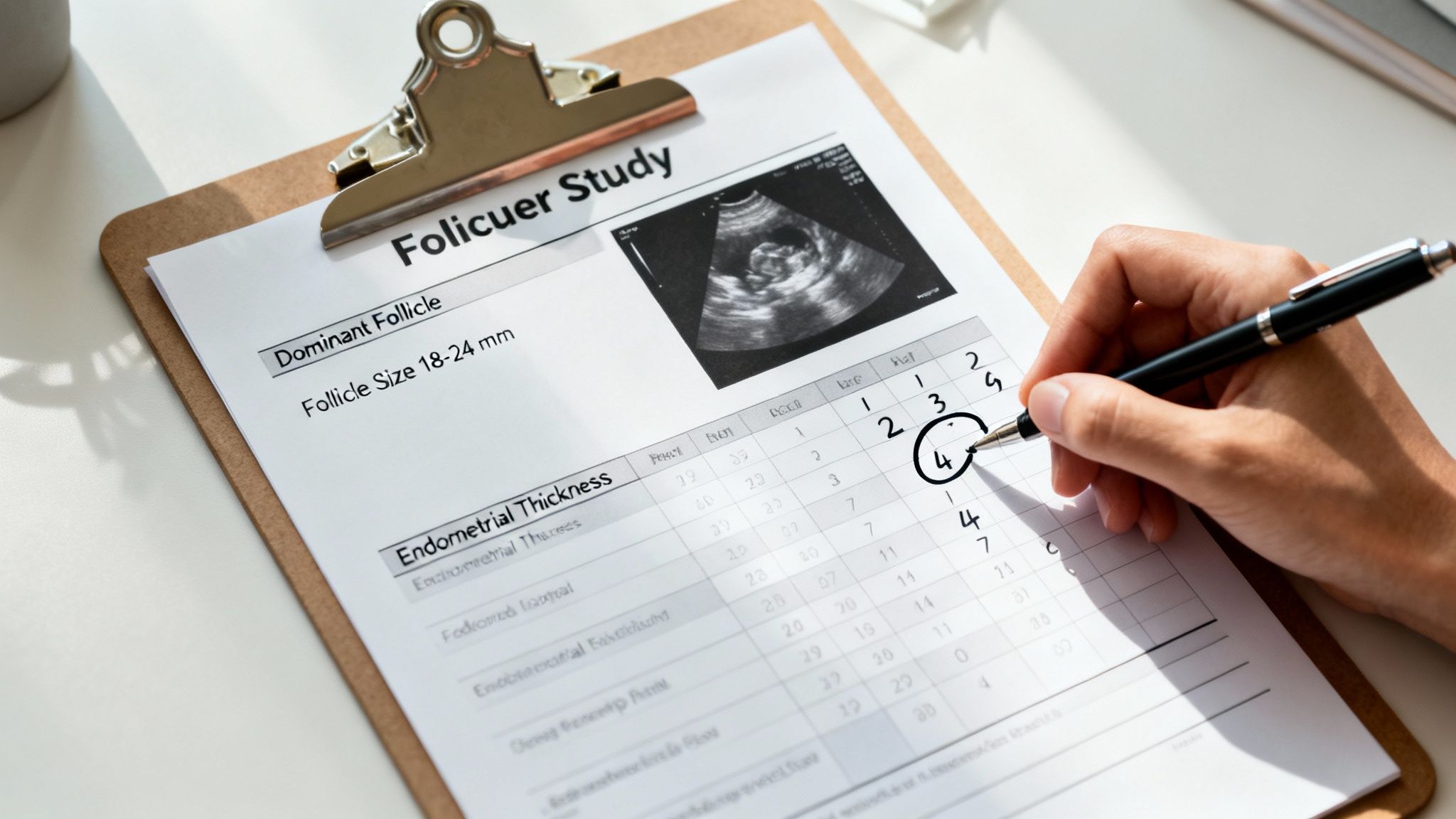
Follicle Growth: In a natural cycle, one follicle will start to grow faster than the rest, becoming the dominant follicle. Your doctor will measure it at every visit. The goal is to see it reach a mature size of about 18-24 mm, which tells us it’s getting ready to release an egg.
Endometrial Thickness: At the same time, the scan measures the lining of your uterus, the endometrium. For a pregnancy to happen, this lining needs to become thick and receptive enough for an embryo to implant.
This simple diagram breaks down the journey into its three core stages: scanning, tracking, and timing for conception.

As you can see, each step builds on the one before it, all aiming to pinpoint the best possible time to conceive.
A follicular study takes the mystery out of ovulation. Instead of guessing, you’re watching it happen. By tracking the lead follicle's growth and the uterine lining's preparation, the process identifies your most fertile window with medical precision.
This careful monitoring continues until that dominant follicle is perfectly mature. Once it hits the right size, we know ovulation is just around the corner, and your best chance for conception has arrived.
How to Read and Understand Your Follicour Study Report
Getting your first follicular study report can feel a bit like trying to read a different language. It’s filled with numbers and medical terms, but don't worry—it’s actually quite straightforward once you know what to look for. Think of it as a progress update on the two most important things happening in your cycle: the growth of your follicles and the health of your uterine lining.
I often tell my patients to picture it like tending a garden. We're watching the main flower bud (the follicle) to see when it will be ready to bloom, while also making sure the soil (your endometrium) is perfectly prepared for a seed to be planted.
The Two Stars of the Show: What Your Report Focuses On
Your report will centre on two key measurements that paint a clear picture of whether your body is getting ready for conception.
Dominant Follicle Size: At the beginning of your cycle, a few follicles will start to grow, but soon enough, one will pull ahead of the pack. This is your dominant follicle, and it’s the one we expect to release an egg. It should grow about 1-2 mm each day, and we're looking for it to reach a mature size, usually somewhere between 18-24 mm.
Endometrial Thickness: This is all about your uterine lining. For an embryo to successfully implant and grow, this lining needs to be thick and welcoming. The goal is to see a thickness of 8 mm or more by the time of ovulation.
You might also see a note about a "triple-line" pattern on your report. This is fantastic news! It’s a sign seen on the ultrasound that shows the endometrium is high-quality and perfectly structured to welcome an embryo.
Follicular Study Milestones in a Typical Cycle
Understanding your report isn't just about a single scan; it's about seeing the progress over time. This table gives you a general idea of what we expect to see at different points in a cycle, helping you follow along with your own results.
Cycle Day | Expected Dominant Follicle Size (mm) | Ideal Endometrial Thickness (mm) |
|---|---|---|
Day 3 | < 10 mm (Antral Follicles) | 2-4 mm |
Day 10 | 12-15 mm | 6-8 mm |
Day 14 (Ovulation) | 18-24 mm | > 8 mm (with triple-line pattern) |
Of course, this is just a guide—every woman's body has its own unique rhythm. The real value of a follicular study is tracking your specific pattern. Research from studies in India has shown just how powerful this tracking is. One analysis found that conception rates were highest when follicles were in the 13–18 mm range, with about 16.7% of all monitored cycles leading to a successful conception.
If you’d like to learn more about what your specific numbers mean, take a look at our detailed guide on decoding your normal follicular study report.
So, Why Has Your Doctor Suggested Follicular Monitoring?
If your doctor has brought up the idea of a follicular study, you might be wondering what it’s all about and why it’s necessary. Think of it less as just another medical procedure and more as a detailed roadmap for your fertility. It’s a way to shift from guessing and hoping to having a clear, data-driven plan.
The single biggest reason? Perfect timing. A follicular study allows your doctor to see exactly what’s happening inside your ovaries and pinpoint your ovulation window with incredible precision. This is crucial for timing intercourse, Intrauterine Insemination (IUI), or In Vitro Fertilisation (IVF) to give you the absolute best chance of success.
But it’s not just about timing. These scans give your doctor a wealth of diagnostic information about the health of your menstrual cycle.
Confirming Ovulation and Checking Your Response
First off, the study confirms whether you’re actually ovulating. It might sound basic, but some women have what are called anovulatory cycles, where no egg is released. Follicular monitoring spots this right away, which is the first step toward finding the right treatment.
This becomes even more important if you’re using fertility medications. The study shows your doctor exactly how your ovaries are responding to the drugs. This real-time feedback is vital for adjusting dosages on the fly, making sure your treatment is effective while also keeping you safe from complications like Ovarian Hyperstimulation Syndrome (OHSS).
A follicular study takes the guesswork out of the equation. It provides a clear, biological picture of what's happening, allowing your medical team to make smart, informed decisions at every stage of your fertility journey.
In India, where infertility impacts an estimated 10-15% of couples, these studies are a fundamental part of fertility care. We know from clinical evidence that follicles measuring between 13-18 mm on the day of an IVF trigger shot are the most likely to lead to a successful pregnancy. In fact, the odds of a live birth go up by 3% for every 10% increase in follicles within this optimal size range. You can read more about these findings in the journal Nature.
As you go through this process, it's also good to know who's on your team. Understanding the difference between a midwife and an obstetrician can help clarify roles in your fertility care. And for those looking at all available options, exploring infertility treatment in Ayurveda can offer a broader perspective on reproductive health.
Connecting the Scans to Your Overall Cycle Health
A follicular study is so much more than just a series of pictures on a screen. It’s a direct window into the intricate hormonal dance that governs your menstrual cycle. What the sonographer sees on the ultrasound—the growing follicles—is the physical result of powerful hormones working tirelessly behind the scenes.
Think of it like watching a flower bloom. The scan lets you see the bud getting bigger and ready to open, but it’s the hormones—like sunlight and water—that are actually making it all happen.
The whole process kicks off with Follicle-Stimulating Hormone (FSH). As its name suggests, this hormone encourages a group of follicles in your ovaries to start maturing. As they grow, these follicles produce oestrogen, which gets to work thickening your uterine lining to create a welcoming home for a potential pregnancy.
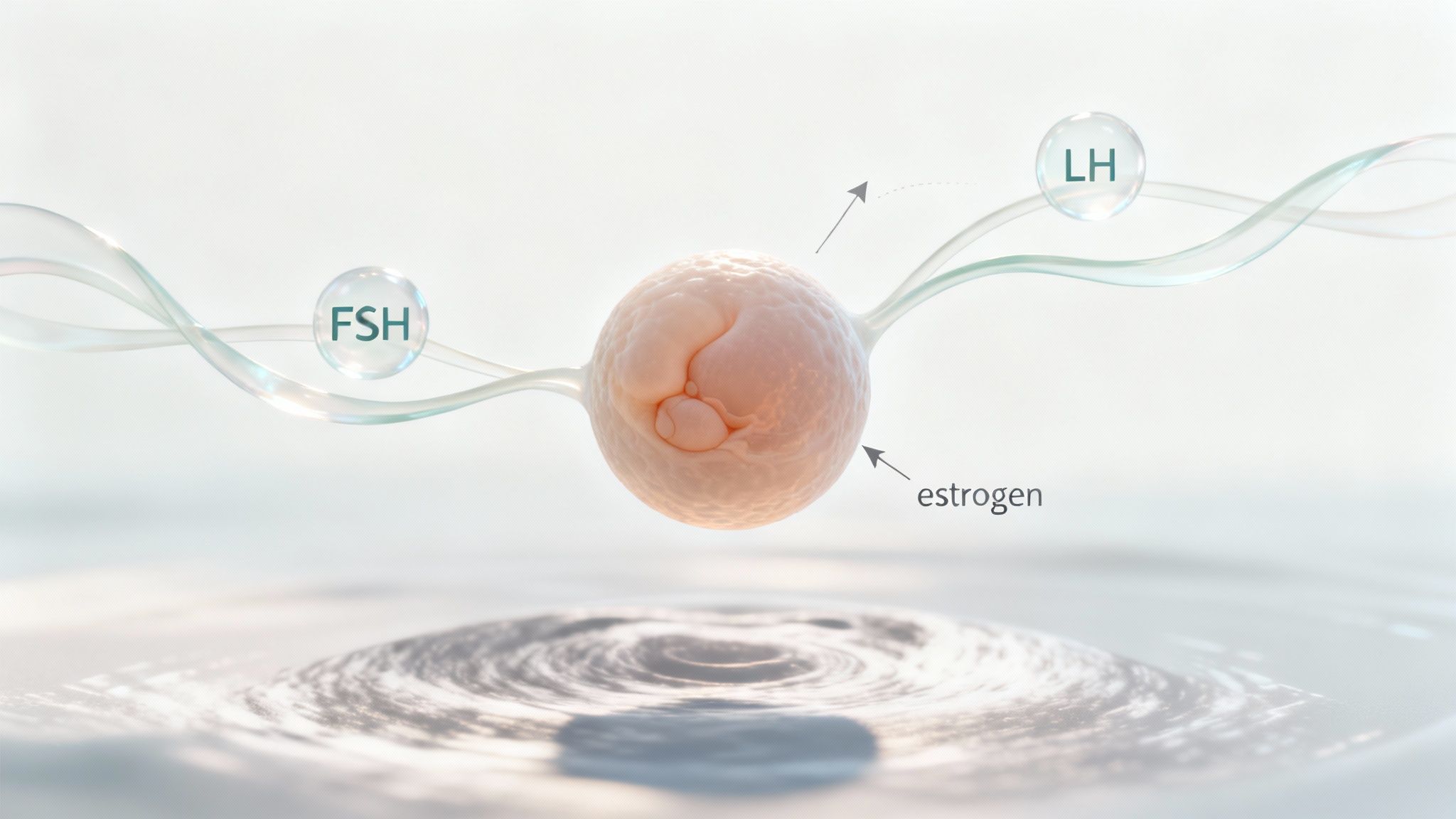
The Final Steps to Ovulation
Once one follicle outpaces the others and becomes the "dominant" one, its oestrogen output hits a peak. This spike sends a signal to your brain, which responds by releasing a surge of Luteinising Hormone (LH). This LH surge is the final trigger, the green light that tells the mature follicle to rupture and release its egg. That moment is ovulation.
Understanding this hormonal cause-and-effect is what gives the follicular study its real power. It’s not just about size; it's about timing. The length of this follicular phase, for instance, is a critical clue to your cycle's health. For Indian women, this phase typically lasts around 12-17 days, though age and individual factors can cause this to vary quite a bit. This is why personalised tracking is so essential.
This holistic view, connecting the physical scans with the hormonal data, shows why a follicular study is such an effective tool. It also underscores the importance of looking after your overall reproductive wellness. To support this journey, you might find it helpful to learn how to improve egg quality naturally for better fertility. And for couples navigating this together, tools that facilitate partner support through period tracking can make the process feel much more collaborative and supportive.
Your Questions About Follicular Studies, Answered
Stepping into the world of fertility treatments can feel overwhelming, and it's completely normal to have a lot of questions. Getting clear answers about what to expect during a follicular study can make the whole process feel less intimidating and put you more in control.
Let's tackle some of the most common concerns head-on.
A big one for many is: does it hurt? The short answer is no. The transvaginal ultrasound (TVS) used for the study might feel a bit awkward or uncomfortable, much like a regular pap smear, but it isn't painful. The probe is small and the whole thing is over in just a few minutes.
Another frequent question is about preparation. The good news is, there’s not much you need to do! You’ll be asked to empty your bladder just before the scan, as this gives the doctor the clearest possible picture of your ovaries. Otherwise, you can go about your day as usual.
What if My Follicles Aren’t Growing?
It’s easy to feel discouraged if a scan shows your follicles aren't developing as hoped, but this is definitely not a dead end. Think of it as valuable information gathering. Your doctor will use these results to figure out why and adjust the plan.
Here’s what might happen next:
Medication Tweaks: If you're on fertility medication, a simple dosage adjustment might be all that's needed for the next cycle.
Deeper Hormone Checks: Your doctor may want to run more detailed blood tests to get a closer look at key hormones like FSH, LH, and oestrogen.
A New Approach: Sometimes, switching to a different type of medication or a completely new protocol can kickstart a better response from your ovaries.
This is why the study is so important—it provides the clues needed to refine your treatment for a better outcome next time.
A follicular study isn't a test you can pass or fail. It's a diagnostic tool. Every cycle, successful or not, gives your doctor critical data to create a more effective, personalised plan for you.
Understanding the Costs Involved
The cost for a full follicular monitoring cycle can differ based on where you are and the clinic you choose. In India, you can typically expect the price for a complete cycle, which includes several scans, to fall somewhere between ₹2,500 and ₹7,000. It's always a smart move to ask your clinic for a detailed breakdown of their package upfront, so there are no surprises.
At JJ Herbals, we believe in supporting your fertility journey with natural, time-tested Ayurvedic solutions. Explore how our organic supplements can complement your path to wellness. Find out more on our website.
.png)
Comments